Sarcoidosis rarely affect patients older than 65 years old. The purpose of this study is to compare and evaluate the demographic, clinical and laboratory features of elderly-onset (EOS) and young-onset sarcoidosis (YOS) patients.
MethodsOne hundred and thirty one patients diagnosed with sarcoidosis according to clinical, radiologic and histopathological evaluation were included in this study. The patients with initial symptoms started after age 65 were accepted as EOS.
ResultsTwenty (15.3%) of 131 patients were diagnosed as EOS, and 111 (84.7%) patients were evaluated as YOS. Fifteen of 20 EOS patients were female and 5 of them were male. Average duration of the disease was determined as 38.4 months for YOS and 22.5 months for EOS (p=0.556). Delay of the diagnosis was 12 months for YOS while it was 3 months for EOS (p=0.001). Higher rates of fatique, comorbid diseases and more hydroxychloroquine (HQ) use were detected in EOS patients comparing to YOS (p=0.010, p=0.003 and p=0.039 respectively).
ConclusionsEOS patients are characterized with higher rates of fatique and comorbid diseases, less inflammatory sign and delayed diagnosis, and less DMARDs use.
La sarcoidosis raramente afecta a mayores de 65 años. Este estudio se diseñó para evaluar las características demográficas, clínicas y de laboratorio de pacientes diagnosticados de sarcoidosis en la tercera edad, comparados con sarcoidosis de inicio en la edad adulta.
Pacientes y métodosCiento treinta y un pacientes fueron diagnosticados de sarcoidosis de acuerdo con la evaluación clínica, radiológica e histopatológica.
ResultadosVeinte pacientes (15,3%) fueron diagnosticados de sarcoidosis en la tercera edad y 111 pacientes (84,7%) fueron diagnosticados en la edad adulta. Quince de los 20 pacientes diagnosticados en la tercera edad eran mujeres y 5 varones. La duración media de la enfermedad fue de 38,4 meses para los pacientes menores de 65 años y de 22,5 meses para los mayores de 65 años. El retraso diagnóstico fue de 12 meses para los primeros y 22,5 meses para los segundos (p=0,001, p=0,010 y p=0,003, p=0,039, respectivamente).
ConclusionesLos pacientes con sarcoidosis de inicio en la tercera edad se caracterizan por mayor incidencia de fatiga y de comorbilidades, menos clínica inflamatoria, menor uso de FAME y mayor retraso diagnóstico.
Sarcoidosis is a systemic disease characterized with a non-caseating granuloma reaction. Although the exact pathogenesis is not clear yet, cellular immune system activation and non-specific inflammatory response occur secondary after exposure to several genetic, infectious and environmental factors.1 Accumulations of Th1 and macrophages with increased production of pro-inflammatory cytokines induce the inflammatory cascade and consecutive impairment in tissue permeability, increase in cellular influx and local cellular proliferation. The main pathological finding of sarcoidosis is non-caseating epitheloid cellular granulomas. Sarcoidosis is a chronic granulomatous disease that may present with various clinical findings. The disease most frequently presents with bilateral hilar lymphadenopathy and infiltrations in the lungs, as well as skin and eye lesions.2 Sarcoidosis have a favorable prognosis, most of the patients are asymptomatic and spontaneous remission rate is more than 60%. Some patients develop chronic progressive disease and mortality rates have been reported in 1–6%. Patients above 40 years of age and black race are associated with worse prognosis.3 Sarcoidosis usually affects the younger population between the ages of 25–40, but 30% of patients may be seen in the elderly population. Elderly-onset sarcoidosis (EOS) is accepted as the onset of disease over 65 years old. Although there is no strict definition of EOS, the most frequently used cut-off age to define ‘elderly’ is the disease onset over 65 years old.4 There are limited and contradictory information in the literature about the incidence and prevalence of EOS based on more case reports and case series.5 Only few studies have examined the clinical features of sarcoidosis in elderly population. The differences between the EOS and young-onset sarcoidosis (YOS) was shown in several studies.6 Constitutional symptoms, specific skin lesions and uveitis are more frequent in EOS than younger patients. When compared with YOS, erythema nodosum or asymptomatic chest X-ray abnormalities are less common in EOS patients.
The aim of our study is to analyze the characteristics and outcomes of patients with EOS and compared them with patients diagnosed at a younger age.
Material and methodOne hundred thirty-one sarcoidosis patients followed-up in a single rheumatology center were retrospectively evaluated. The patients who had initial symptoms onset after 65 years old were accepted as EOS. All of the patients were divided into two groups as EOS and YOS and were compared in terms of1: demographic and epidemiological data (age, gender, duration of disease, delay in diagnosis)2; clinical features (fatique, uveitis, arthritis, skin involvement, etc.)3; laboratory data (acute phase reactants, serum angiotensin converting enzyme (ACE), calcium, etc.)4; radiological data (stage)5; drug usage6; outcomes. Detailed medical histories of the patients were obtained, and their systemic and locomotor system examinations were completed. Sarcoidosis diagnosis were made through clinical, laboratory, imaging and histopathological investigations. Demonstration of noncaseating granulomas were shown on pathological specimen (except for patients presenting with Löfgren syndrome, for whom the diagnosis of sarcoidosis was made without requiring histological evidence). Other factors (tuberculosis, bacterial and fungal infections) that may cause granulomatous diseases were ruled out. All patients were evaluated and checked for existence of comorbid diseases (hypertension, diabetes, coronary artery disease). Laboratory investigations were performed; routine biochemistry, acute phase reactants (erythrocyte sedimentation rate (ESR), C-reactive protein (CRP)), serum ACE, calcium and hydroxy-vitamin D3 levels were checked. Chest X-ray and thorax computed tomography (CT) were performed for staging of sarcoidosis. The approval ethics statement was not required in accordance with the policy of our institution.
Statistical analysisData was analyzed by statistical package for the social sciences (SPSS) 20.0 software for Windows statistical package (SPSS, Chicago, Illinois, USA). Categorized data was cross tabled and tested with Chi-square test. Numeric variables, which change in normal ranges were analyzed with t-test, abnormally ranged variables were analyzed with Mann Whitney-U test. Pearson correlation coefficients for variables with normal distribution were used. Statistical significance threshold value was 0.05.
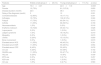
ResultsTwenty (15.3%) of 131 patients were diagnosed as EOS, and 111 (84.7%) patients were evaluated as YOS. Fifteen of 20 EOS patients were female and 5 of them were male. Average duration of the disease was determined as 38.4 months for YOS and 22.5 months for EOS (p=0.556). Delay of the diagnosis was 12 months for YOS while it was 3 months for EOS (p=0.001). Female predominance, erythema nodosum, and uveitis were determined to be more frequent in EOS group, but this was not statistically significant (p=0.850, p=0.628 and p=0.859 respectively). Higher rates of fatique, comorbid diseases and more Hydroxychloroquine (HQ) use were detected in EOS patients compared with YOS (p=0.010, p=0.003 and p=0.039 respectively). Compared with YOS patients less arthralgia, Löfgren's syndrome and less delay in diagnosis were detected in EOS patients. Higher levels of elevated serum ACE level and ESR were determined in the EOS group as compared to YOS group, but this was not statistically significant. There was no significant difference in terms of radiologic stage of disease. The incidence rate of specific skin lesions, myopathy and bone involvement were also similar for both groups (p=0.670, p=0.670, p=0.670 respectively). When compared both groups in terms of musculoskeletal system involvement, there was not statistically significant differences (p=0.709). The use of non-steroidal anti-inflammatory drugs, corticosteroids, azathyoprin, methotrexate and colchicine were similar in both groups, but there was a more frequent HQ use in EOS group (p=0.039) (Table 1). In term of mortality, one of the 20 patients in the EOS group died from myocardial infarction, while there was not any death in the YOS group. The 3-year survival rate after diagnosis of sarcoidosis was 95% in the EOS group, compared with 100% in the YOS group.
Comparison between young and elderly onset sarcoidosis patients according to demographic, clinical and laboratory features.
| Features | Elderly-onset group (n=20) (%) | Young-onset group (n=111) (%) | p-value |
|---|---|---|---|
| Age | 70.3±3.37 | 44.9±11.9 | 0.0001 |
| Female | 15 (75%) | 81 (%72.9) | 0.850 |
| Disease duration (month) | 22.5 | 38.4 | 0.013 |
| Delay of the diagnosis (month) | 3 | 12 | 0.001 |
| Comorbid diseases | 12 (60%) | 19 (17.1%) | 0.001 |
| Arthralgia | 15 (75%) | 102 (91.9%) | 0.024 |
| Fatique | 17 (75%) | 60 (54.1%) | 0.010 |
| Arthritis | 11 (55%) | 66 (59.5%) | 0.709 |
| Neurosarcoidosis | 1 (5%) | 0 (0%) | 0.018 |
| Erythema nodosum | 10 (%50) | 49 (44.1%) | 0.628 |
| Lupus pernio | 0 (0%) | 1 (0.9%) | 0.670 |
| Löfgren syndrome | 1 (5%) | 18 (16.2%) | 0.019 |
| Myopathy | 0 (0%) | 1 (0.9%) | 0.670 |
| Uveitis | 3 (20%) | 15 (13.5%) | 0.859 |
| Bone involvement | 0 (0%) | 1 (0.9%) | 0.670 |
| Elevated serum ACE | 11 (55%) | 48 (43.2%) | 0.331 |
| Elevated serum ESR | 11 (55%) | 55 (49.5%) | 0.654 |
| Elevated serum CRP | 8 (40%) | 50 (45%) | 0.676 |
| CS use | 4 (20%) | 40 (36%) | 0.162 |
| NSAIDs use | 11 (55%) | 53 (47.7%) | 0. 550 |
| HQ use | 5 (25%) | 10 (9%) | 0.039 |
| MTX use | 0 (0%) | 3 (2.7%) | 0.457 |
| AZA use | 0 (0%) | 1 (0.9%) | 0.670 |
| CD use | 1 (5%) | 3 (2.7%) | 0.583 |
Abbreviations: CE, angiotensin converting enzyme; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; CS, corticosteroids; NSAIDs, non-steroidal antiinflammatory drugs; HQ, hydroxychloroquine; MTX, methotrexate; AZA, azathyoprine; CD, colchicum dispert.
In this study, we examined the demographic, clinical and laboratory data of patients with EOS. Compared with YOS patients, EOS patients have more general symptoms, comorbid conditions and HQ use. Additionally less Löfgren syndrome, delay in diagnosis and less use of DMARDs was seen in EOS patients. We have not found any statistically significant differences when compared two groups regarding other clinical, laboratory and radiological parameters (uveitis, skin lesion, CRP etc.). There are limited and conflicting data in the literature about the EOS characteristics, usually based on case reports and retrospective studies. Chevalier et al. shared the data of 30 EOS patients, followed in single institution between 1986 and 2000 years. Compared with YOS, more constitutional symptoms (fatigue, weakness, tiredness), intrathoracic involvement, and corticosteroids use were found in EOS patients while no difference was observed in respect to disease prognosis.7 Varron et al. compared the YOS and EOS cases and showed that asthenia, uveitis, and specific skin lesions are more frequent in patients with EOS.8 Another study reported that sarcoidosis clinical symptoms and organ involvement are similar between both groups.9 In a study performed in our country, extrapulmonary involvement was observed more common in EOS patients while less Löfgren syndrome, erythema nodosum and uveitis has been reported.10 Sarcoidosis is a heterogeneous disease which may present with different clinical findings.11 While the most common presentation is intrathoracic involvement, extrapulmonary (eyes, skin, heart, locomotor system, etc.) involvements may also occur. Although may be seen in all age groups, sarcoidosis is most frequently seen between the ages of 25–45. Second peak of the disease was reported in postmenopausal women from Northern European countries.12 EOS is a rare entity and increased female predominance may observed in this age group. Female/male ratio was 1/1 in YOS, while in EOS appears to be the ratio of 5/1. These data suggest that hormonal factors have an influence on the activity of sarcoidosis.13 The constitutional symptoms dominate the clinical features in the elderly population while the classical sarcoidosis symptoms (erythema nodosum, typical radiological findings, etc.) may be in the background. Fatigue, weight loss and general state disorder symptoms is more common in EOS patients and may mimic malignancies. In our cohort, general symptoms (fatique, weakness) were dominated while the classical symptoms (such as Löfgren syndrome, uveitis, arthritis etc.) were observed less common. Because comorbid conditions are more frequent in EOS, diagnosis, differential diagnosis and treatment strategies might be more difficult. However, the presence of comorbid diseases might affect the prognosis of sarcoidosis. It is speculated that patients with EOS and comorbid disease might have worse prognosis.14 According to our study results, the EOS patients have more comorbid diseases and worse outcome than YOS patients. When compared in terms of treatment options, corticosteroids seem to be the first choice in both sarcoidosis groups. However, some studies suggest that the drug side effect profile is higher in EOS patients.15 In our cases, corticosteroids were used as fırst drug in both groups, whereas as DMARDs use HQ were preferred in EOS patients.
Our study has some limitations. First, the study was a retrospective comparative study. Because of this, data for some of the clinical and laboratory investigations were missing in both groups. It is likely that a prospective study would provide much clearer and more complete information. Secondly the study was performed at a single institution. Because of the single-center data, the results obtained from this work prevent us from making a generalization for all Turkish EOS patients.
In conclusion, elderly-onset sarcoidosis have different characteristics compared to young-onset sarcoidosis. Female predominance, general symptoms, comorbid diseases and HQ use are more frequent in EOS, while Löfgren syndrome, delayed diagnosis and DMARDs use are less common. There are similarities in terms of disease course and treatment options, but comorbid disease presence may be a risk factor for EOS prognosis. Multicenter, prospective studies are needed to confirm our results.
Conflict of interestThe authors declared not any conflict of interest or any financial support.