Rheumatoid arthritis (RA) is a chronic inflammatory disease characterized by swelling, tenderness and destruction of synovial joints, leading to severe disability and premature mortality. The aim of the study was to determine the diagnostic accuracy of the 3 isotypes of rheumatoid factor (RF), anti-citrullinated peptide antibodies (ACPA) and the combination of both, for the diagnosis of rheumatoid arthritis (RA) in non-selected patients with inflammatory arthralgia.
MethodsWe include 129 patients with inflammatory Arthalgia from a third level reference Center of rheumatic diseases in Monterrey, México. Their samples were analyzed for RF isotypes (IgA, IgG, and IgM) by ELISA (EUROINMUN), using a cut-off of 20IU/ml, and for ACPA's 5IU/ml; a medical examination was performed to obtain the definitive diagnoses of the patients. Data analysis was carried out using ROC curves for the measurement of sensitivity, specificity, for diagnostic accuracy to verify if the use of 3 RF isotypes and ACPA had a better prediction for the diagnosis of RA than use only one isotype and the ACPA alone.
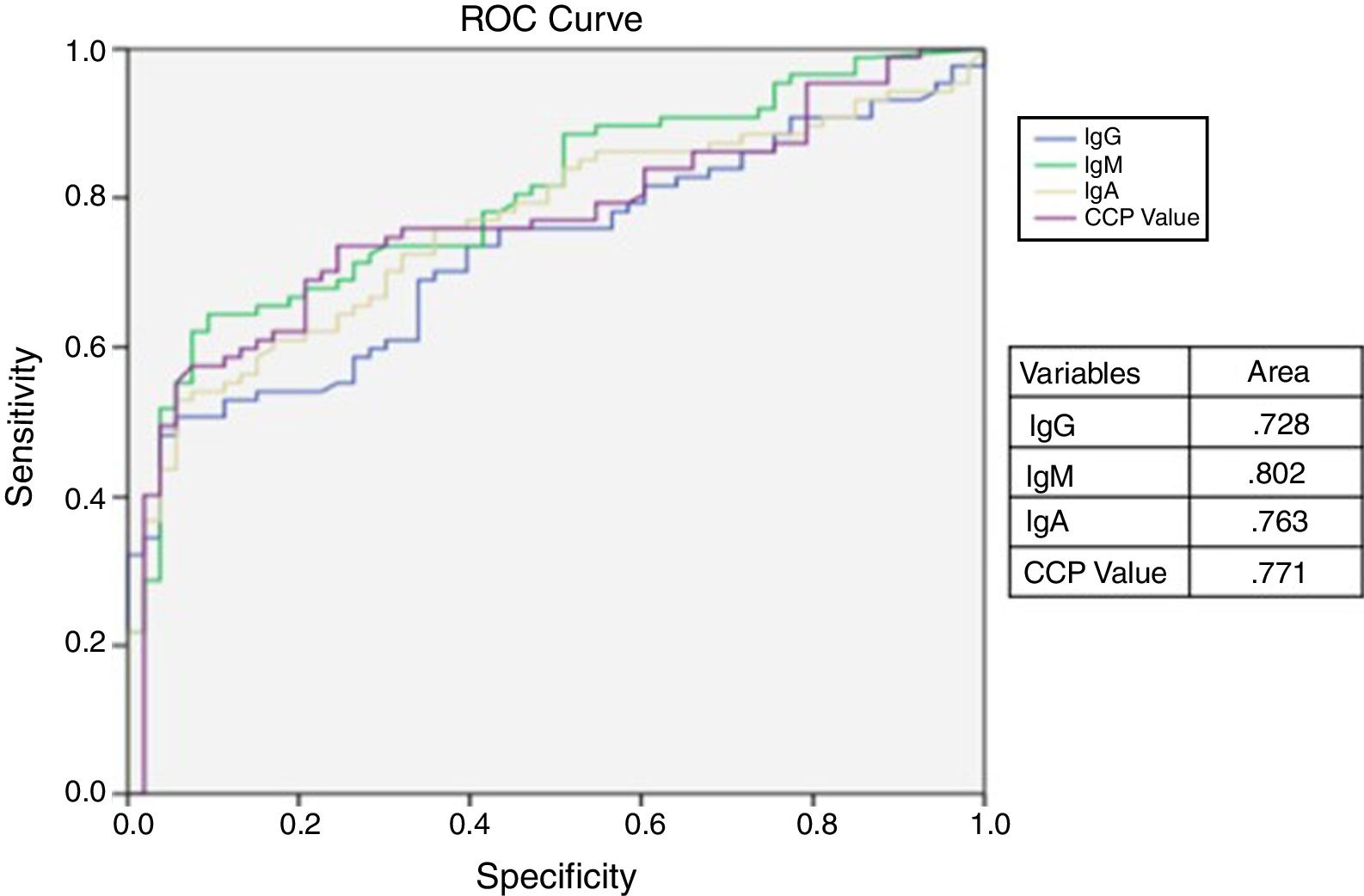
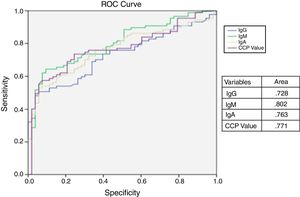
ResultsThe ROC showed a sensitivity and specificity of the different antibodies with different cut-off points, being the best for the IgM with 0.802 followed by ACPA, IgA and IgG with 0.771, 0.63, and 0.728 respectively without statistical difference, the sensitivity and specificity of the combination of the 4 antibodies were 81.4 and 73.66%.
ConclusionIn non-selected patients with inflammatory arthralgia, the combination of ACPA and isotypes of RF did not demonstrate more sensibility and specificity than IgM isoform of rheumatoid factor measurement only. We recommend that in the clinical scenario of arthralgia, where the diagnoses are Lupus, Sjogren syndrome and Osteoarthritis, RF IgM isoform is used followed by ACPA.
La artrtitis reumatoide (AR) es una enfermedad inflamatoria crónica caracterizada por inflamación, sensibilidad y destrucción de la membrana sinovial de las articulaciones, dando lugar a una discapacidad grave y mortalidad prematura. El objetivo del estudio fue determinar la precisión diagnóstica de los 3 isotipos del factor reumatoide (RF), los anticuerpos peptídicos anti citrulinados (ACPA) y la combinación de ambos, para el diagnóstico de AR en pacientes no seleccionados con artralgia inflamatoria.
MétodosFueron incluidos 129 pacientes con artralgia inflamatoria de un centro de referencia de enfermedades reumáticas de tercer nivel en Monterrey, México. Sus muestras se analizaron para determinar los isotipos de RF (IgA, IgG e IgM) mediante ELISA (Euroinmun), usando un límite de 20UI/ml, y de 5UI/ml de ACPA. Se realizó un examen médico para obtener los diagnósticos definitivos de los pacientes. El análisis de los datos se realizó mediante las curvas ROC para la medición de la sensibilidad, la especificidad y la precisión diagnóstica para verificar si el uso de 3 isotipos de RF y ACPA tenía una mejor predicción para el diagnóstico de la AR que el uso de un solo isotipo y el ACPA solo.
ResultadosLa curva ROC mostró una sensibilidad y especificidad de los diferentes anticuerpos con diferentes puntos de corte, siendo el mejor para el IgM con 0,802 seguido de ACPA, IgA e IgG con 0,771, 0,63 y 0,728, respectivamente, sin diferencia estadística; la sensibilidad y la especificidad de la combinación de los 4 anticuerpos fueron 81,4 y 73,66%.
ConclusiónEn pacientes no seleccionados con artralgia inflamatoria, la combinación de ACPA e isotipos de RF no demostró más sensibilidad y especificidad que la isoforma IgM de la medición del RF solamente. Recomendamos que, en el escenario clínico de artralgia, donde los diagnósticos son lupus, síndrome de Sjögren y osteoartritis, se use la isoforma RF IgM seguida de los ACPA.
Rheumatoid arthritis (RA) is a chronic inflammatory disease characterized by swelling, tenderness and destruction of synovial joints, leading to severe disability and premature mortality. The impact of early diagnosis and treatment of inflammatory arthropathies is widely demonstrated as well as the prognostic value of immunological markers.1
ACR/EULAR 2010 classification criteria require autoimmunity and acute phase reactants presence to establish RA diagnosis/classification.1 Criteria specifies, that the rheumatoid factor (RF) isotype should be IgM, to be considered a positive criterion. Although it has been reported that the presence of IgG (19.3%) and IgA (33.7%) RF's isotypes are present in RA patients before diagnosis,2 it is unknown whether the use of different RF isotypes as autoimmunity markers adds some value to the diagnosis in unselected patients with inflammatory arthralgia where RA is suspected in real life case scenario.
The aim of the study was to determine the diagnostic accuracy of the 3 RF isotypes and anticitrullinated peptide antibodies (ACPA) alone, and in combination in the diagnostic confirmation of RA in non-selected patients with inflammatory arthralgia.
MethodPopulation of studyWe performed an observational, transversal and diagnostic test study. We include 129 patients older than 18 years, with hand inflammatory arthralgia, which were evaluated in a University Hospital, and had requested autoimmunity test confirmation in a central laboratory, in Monterrey, México from March 2014 to March 2015. We excluded patients with any confirmed inflammatory arthritis diagnosis at the time of laboratory test, including RA, psoriatic arthritis, systemic lupus erythematosus, primary Sjögren syndrome. Patient serum samples were sent to the rheumatology laboratory for the measurement of the three RF isotypes and ACPA. The ethics committee, with registration number RE15-011, approved this study. The collection of clinical and laboratory data was performed from the clinical charts. The final diagnosis was established in a second appointment by certified rheumatologist, after reviewing of the clinical and laboratory data in a 2 weeks period after laboratory was performed. The SLE diagnosis was established in based of clinical grounds and autoimmune demonstration of specific antibodies. The SS diagnosis was established based of clinical grounds, specific antibodies and minor salivary gland biopsy. And osteoarthritis diagnosis was established in clinical, laboratory and radiological grounds.
ImmunoassaySamples were analyzed for RF immunoglobulin isotypes (IgA, IgG, and IgG) by ELISA (EUROINMUN in IU/ml, using a cutoff point of 20IU/ml), and ACPA by ELISA (EUROINMUN in IU/ml, cutoff of 5UI/ml).
Statistical analysisA categorical descriptive analysis was carried out with frequencies and percentages and for the numerical variables we used means with standard deviation (SD) or median and interquartile ranges (IQR), after Gaussian distribution was established. We calculate sensitivity and specificity of each antibody and its combination for the diagnosis of RA against another inflammatory arthralgia, finally the ROC curve was calculated by the diagnostic accuracy of each antibody.
ResultsSixty-two (44.3%) patients were finally diagnosed with RA, and 67 (55.7%) of the patients were classified as non-RA patients. The non-RA group final diagnosis consisted of 10 (7.1%) with Primary Sjögren Syndrome (pSS), 5 (3.5%) with Systemic Lupus Erythematosus (SLE) and 52 (37.1%) with hand osteoarthritis (OA).
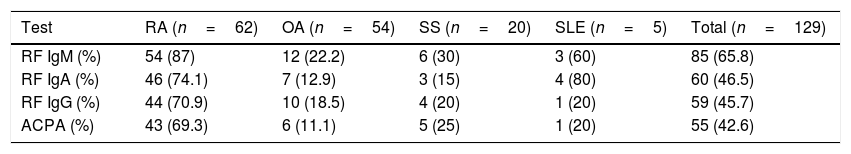
Prevalence of autoimmunity in RA patients were as follows: 54 (87.0%) were positive for IgM RF, 46 (74.1%) were positive for IgA RF, 44 (70.9%) were positive for IgG RF and 43 (69.3%) were positive for ACPA, the positivity frequencies of the group of patients without RA are shown in Table 1.
Autoantibodies frequency by disease.
| Test | RA (n=62) | OA (n=54) | SS (n=20) | SLE (n=5) | Total (n=129) |
|---|---|---|---|---|---|
| RF IgM (%) | 54 (87) | 12 (22.2) | 6 (30) | 3 (60) | 85 (65.8) |
| RF IgA (%) | 46 (74.1) | 7 (12.9) | 3 (15) | 4 (80) | 60 (46.5) |
| RF IgG (%) | 44 (70.9) | 10 (18.5) | 4 (20) | 1 (20) | 59 (45.7) |
| ACPA (%) | 43 (69.3) | 6 (11.1) | 5 (25) | 1 (20) | 55 (42.6) |
RA: rheumatoid arthritis, ACPA: anti-citrullinaed peptide antibodies, RF: rheumatoid factor, SS: Sjögren's syndrome, Ig: inmmunoglobulin, SLE: systemic lupus eritematosus, OA: osteoarthritis.
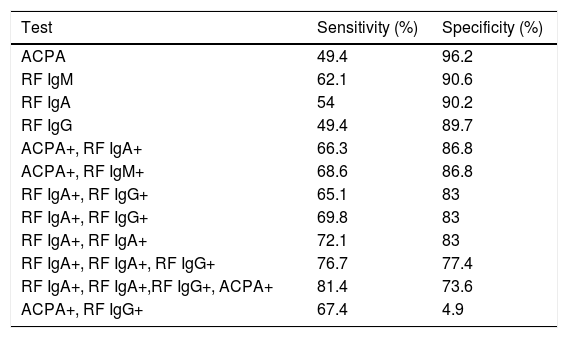
The sensitivity and specificity for RA diagnosis were as follows: 49.4% and 96.2% for ACPA, 62.1% and 90.6% for IgM RF, 54% and 90.6% for IgA RF, 49.4% and 89.7% for IgG RF, and for the positivity combination of IgM, IgG, IgA RF and ACPA were 81.4% and 73.6%, respectively. The sensitivity and specificity of the antibody combination for RA diagnosis are depicted in Table 2. The incremental addition of antibodies does not improve specificity but increases sensitivity.
Sensitivity and specificity according to autoantibodies for RA detection.
| Test | Sensitivity (%) | Specificity (%) |
|---|---|---|
| ACPA | 49.4 | 96.2 |
| RF IgM | 62.1 | 90.6 |
| RF IgA | 54 | 90.2 |
| RF IgG | 49.4 | 89.7 |
| ACPA+, RF IgA+ | 66.3 | 86.8 |
| ACPA+, RF IgM+ | 68.6 | 86.8 |
| RF IgA+, RF IgG+ | 65.1 | 83 |
| RF IgA+, RF IgG+ | 69.8 | 83 |
| RF IgA+, RF IgA+ | 72.1 | 83 |
| RF IgA+, RF IgA+, RF IgG+ | 76.7 | 77.4 |
| RF IgA+, RF IgA+,RF IgG+, ACPA+ | 81.4 | 73.6 |
| ACPA+, RF IgG+ | 67.4 | 4.9 |
ACPA: anti-citrullinated peptide antibodies, RF: rheumatoid factor, Ig: immunoglobulin.
The ROC curve analysis was performed to calculate the area under the curve (AUC). The curve shows the sensitivity and specificity of the antibodies with different cut-off values. The best AUC was for RF IgM with 0.802 (0.718–0.868, 95% CI) followed by ACPA, IgA RF and IgG RF with 0.771 (0.685–0.848, 95% CI), 0.763 (0.672–0.834, 95% CI), and 0.728 (0.672–0.833, 95% CI) respectively, but with not statistical difference, demonstrated by the confidence intervals (Fig. 1).
DiscussionWe found a sensitivity of 62.1% and a specificity of 90.6% for IgM-RF (which is the most used and criteria recommended) followed by a sensitivity of 49.4% and a specificity of 96.2% for ACPA in unselected inflammatory arthralgia patients. Chang et al. reported 67% sensitivity and 79% specificity of IgM RF and 79% sensitivity and 98% specificity for ACPA.3 This difference could be explained because different inclusion criteria of patients evaluated in each study. In our study the patients were non-selected inflammatory arthralgia patients, who had not definite diagnosis. In Chang study, they selected a population with previous RA diagnosis, classified by 1987 ACR criteria, the present study was performed in population in study protocol without confirmed diagnosis, that could explain the changes in the sensitivity and specificity of the test.
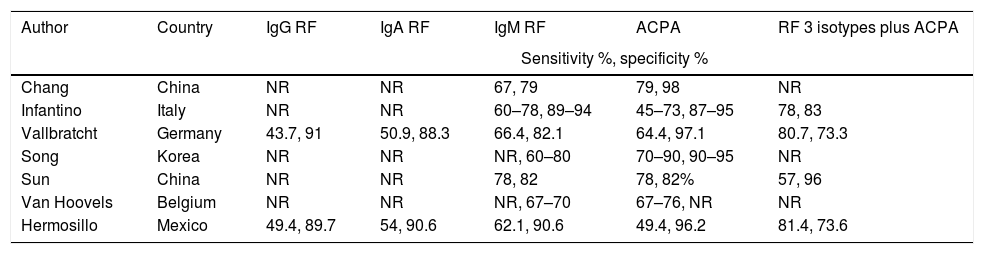
In Table 3, we describe the different approaches to RF and ACPA diagnostic performances by different authors.
Different approaches to diagnostic performance of RF and ACPA.
| Author | Country | IgG RF | IgA RF | IgM RF | ACPA | RF 3 isotypes plus ACPA |
|---|---|---|---|---|---|---|
| Sensitivity %, specificity % | ||||||
| Chang | China | NR | NR | 67, 79 | 79, 98 | NR |
| Infantino | Italy | NR | NR | 60–78, 89–94 | 45–73, 87–95 | 78, 83 |
| Vallbratcht | Germany | 43.7, 91 | 50.9, 88.3 | 66.4, 82.1 | 64.4, 97.1 | 80.7, 73.3 |
| Song | Korea | NR | NR | NR, 60–80 | 70–90, 90–95 | NR |
| Sun | China | NR | NR | 78, 82 | 78, 82% | 57, 96 |
| Van Hoovels | Belgium | NR | NR | NR, 67–70 | 67–76, NR | NR |
| Hermosillo | Mexico | 49.4, 89.7 | 54, 90.6 | 62.1, 90.6 | 49.4, 96.2 | 81.4, 73.6 |
ACPA: anti-citrullinated peptide antibodies, RF: rheumatoid factor, Ig: immunoglobulin, NR: not reported.
Infantino et al. found that the best combination for screening was the combination of ACPA plus IgA and IgM RF in an early arthritis patient.4 We observed that the best combination for screening was use of 4 antibodies.
Vallbracht et al.5 describe in a prospective study in 715 arthralgia patients, that the best screening method for RA was the combination of IgM RF and ACPA compared to other RF isotypes, clarifying the importance of ACPA measurement for early diagnosis in patients with negative RF.
It is important to note that our patients had inflammatory arthralgia and not a diagnosis of RA. It is well known that most auto antibodies tend to increase and peak at the onset of disease,6 but we may find low titers in the early stages of the disease. Therefore, the addition of RF to ACPAs will add sensitivity for the diagnosis of RA in patients with inflammatory polyarthralgia.7
The performance of the combination of the 3 isotypes of RF and ACPAs for RA diagnosis showed a sensitivity of 81.4% and a specificity of 73.6% in patients with inflammatory arthralgia. Comparing the combination with the single test that performed the best individually, which was RF-IgM with a sensitivity of 62.1% and a specificity of 90.6%.8 The sensitivity increased considerably but with a decrease in specificity. Unlike ACPA, RF specificity is limited because it is also detected in other diseases as well as in healthy individuals. The sensitivity of a test may be an important factor to consider when evaluating patients with polyarthritis of an autoimmune origin is sought to obtain the definitive diagnosis. The specificity (confirmatory characteristic of a test) is greater for ACPA alone, which had a decrement, when added to RF's, given the non-RA groups diagnosis (SLE, Sjögren). The RF's cut-off provided by the manufacturer is low and very sensitive, as long as the derivation cohorts included healthy participants. When we explored the in the ROC for ACPA a better sensitive and specific cut-off different from the manufacturer, we found that 10UI/dL had 61% sensitivity and 80% specificity.
In the real-life case scenario of inflammatory arthralgia, in patients where we suspect of RA diagnosis, the IgM RF and ACPA continue being the best options to classify RA.
Van Hoovels et al. documented an increase in RF positivity when the EUROIMMUN kit was used. Also showed low concordance compared with 6 other diagnostic kits used in daily clinical practice for the detection of these antibodies.9 We consider that this increase in sensitivity test, in addition to the high prevalence of rheumatoid factor in non-rheumatic joint diseases, caused the high prevalence of positive isotypes of the RF and ACPA in patients without RA.
ConclusionsIn patients non-selected with Inflammatory arthralgia the combination of ACPA and RF isotypes do not demonstrate more sensitivity and specificity than IgM RF alone. Its use routinely in combination could cause an increase of false positives in healthy patients or with an immunological condition different from rheumatoid arthritis. The diagnostic performance of a test is resumed in the AUC of the ROC, even thought, IgM RF isotype had the greatest one; it did not differ statistically from others. In a high pre-test probability clinical scenario, ACPA had better specificity to confirm RA, nonetheless, the addition of all RF isotypes did not add diagnostic performance.
The search of autoimmunity with low specificity unnecessary autoantibodies expose the patients to unnecessary treatments. We recommend that in the clinical scenario of inflammatory arthralgia, where the differential diagnoses include SLE, SjS and osteoarthritis, RF IgM isotype and ACPA are more useful to confirm RA diagnosis.
FundingNeither the research, nor the authors received any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of InterestNone declared.